Bone screws are critical components in orthopedic fixation systems, providing stability in fracture repair, spinal fusion, and reconstructive surgeries. Their performance depends on design features, material properties, mechanical strength, and surgical handling. This comprehensive overview examines screw types, material specifications, mechanical testing, surgical techniques, complications, quality standards, and application-specific performance data.
Types of Bone Screws
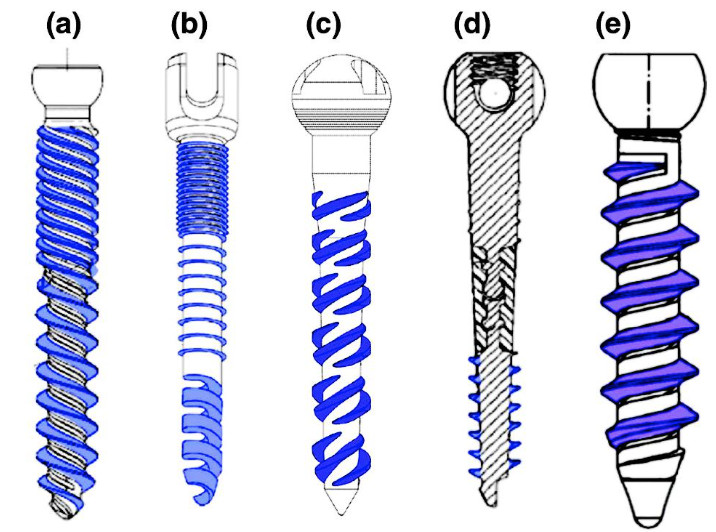
Bone screws can be broadly classified based on thread design, head configuration, and intended anatomical application. Selection depends on bone density, load requirements, and implant location.
| Type | Thread Profile | Head Style | Typical Diameter (mm) | Length Range (mm) | Primary Application |
|---|---|---|---|---|---|
| Cortical Screw | 0.5 mm pitch, V-profile | Hexagonal/Slotted | 2.0–4.5 | 10–60 | Dense cortical bone fixation |
| Cancellous Screw | 1.25 mm pitch, deep V-profile | Hexagonal/ Torx | 4.0–7.3 | 20–100 | Spongy cancellous bone |
| Locking Screw | Self-tapping, coarse pitch | Low-profile, Suture eyelet | 3.5–6.5 | 20–90 | Plate–screw locking constructs |
| Lag Screw | Partially threaded | Flat or countersunk | 3.0–6.5 | 15–80 | Interfragmentary compression |

Design and Material Specifications
Material choice influences biocompatibility, corrosion resistance, modulus of elasticity, and fatigue life. Titanium alloys and stainless steels are most common; bioresorbable polymers and magnesium alloys are emerging solutions in specific applications.
- Titanium Alloy (Ti-6Al-4V ELI): Yield strength ≥ 795 MPa, elastic modulus ~110 GPa, corrosion resistance in physiological saline, non-magnetic.
- 316L Stainless Steel: Yield strength ~290 MPa, elastic modulus ~200 GPa, good machinability, potential for nickel release.
- PLLA/PDLLA (Poly-L-lactic acid): Tensile strength 50–100 MPa, modulus 2–4 GPa, complete resorption in 12–18 months, acidic degradation products.
- Magnesium Alloys (Mg-Zn-Ca): Yield strength 150–200 MPa, elastic modulus ~45 GPa, bioresorbable, rapid corrosion concerns without proper coatings.
Mechanical Properties and Testing
Mechanical integrity is assessed through static and dynamic tests, measuring pull-out strength, torsional strength, and bending fatigue. Test protocols follow ASTM F543 and ISO 10993 series for biocompatibility.
| Parameter | Cortical Titanium Screw | Cancellous Stainless Steel | PLLA Resorbable Screw |
|---|---|---|---|
| Pull-out Strength (N) | 1500–2000 | 800–1200 | 300–500 |
| Torsional Strength (N·m) | 4.5–6.0 | 3.0–4.0 | 1.0–1.5 |
| Fatigue Life (cycles @ 50 % UTS) | >&106 | >5 × 105 | Not specified |
| Shear Strength (MPa) | 900–1100 | 600–800 | 50–80 |
Dynamic fatigue testing under axial bending follows ASTM F1717 for anterior spinal constructs. Measurements include load to failure, cycles to 2 mm displacement, and stiffness retention after simulated body fluid immersion.
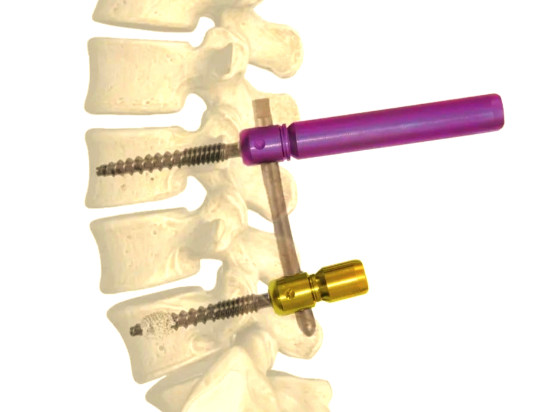
Surgical Techniques and Installation
Correct surgical handling ensures optimal primary stability and reduces peri-implant complications. Steps include pre-operative planning, pilot hole drilling, screw insertion, and torque control.
- Pilot Hole Preparation: Drill diameter 0.5 mm less than screw minor diameter for cancellous bone; use cortical drill bits for cortical screws.
- Thread Cutting vs. Self-Tapping: Self-tapping screws reduce operative steps but generate higher insertion torque; pre-tap threads in dense cortical bone to avoid microfractures.
- Insertion Torque: Monitor with torque-limiting driver; typical ranges:
- Cortical screw: 1.5–3.0 N·m
- Cancellous screw: 0.75–1.5 N·m
- Torque Limitation: Over-tightening risks thread stripping and bone necrosis; under-tightening compromises fixation strength.
- Compression and Lag Technique: Countersink head below cortical surface, engage near cortex, then compress far fragment for interfragmentary stability.
Complications and Considerations
Several clinical hurdles can compromise outcomes, requiring detailed assessment and management strategies.
- Pull-Out Failure: Low bone density or undersized screws increase risk. Consider augmentation with polymethylmethacrylate (PMMA) or hydroxyapatite-coated screws.
- Stress Shielding: High-modulus materials can lead to periprosthetic bone resorption. Selection of lower modulus alloys or resorbable screws may mitigate this effect.
- Corrosion and Ion Release: Stainless steel may release Ni and Cr in corrosive environments. Titanium alloys exhibit better passivation but can suffer fretting corrosion at screw–plate interfaces.
- Thermal Necrosis: Drilling speeds > 1500 rpm without irrigation can raise local temperatures above 47 °C, causing bone cell death. Maintain irrigation flow rate ≥ 50 mL/min.
- Biodegradation Control: Resorbable materials degrade by hydrolysis; rate can be accelerated in acidic microenvironment. Coatings or blended polymer matrices help regulate degradation time.
Quality Control and Standards
Manufacturers must comply with international standards to ensure safety and performance consistency. Key standards include:
- ASTM F543: Standard Specification and Test Methods for Metallic Bone Screws.
- ISO 5835: Implants for surgery — Bone screws with conical and cylindrical heads.
- ISO 10993 Series: Biological evaluation of medical devices.
- ISO 13485: Quality management systems for medical device manufacturing.
Inspections include dimensional verification (±0.02 mm tolerance), surface finish (Ra ≤ 0.8 µm), mechanical test reports, and certificate of biocompatibility. Batch traceability is maintained via laser-etched lot numbers.
Applications and Performance Data
Bone screws are used across multiple orthopedic domains. Representative application performance metrics are summarized below.
- Spinal Fixation: Pedicle screws achieve pull-out forces > 2000 N in lumbar vertebrae with augmentation. Fatigue life under 10 Nm bending exceeds 1 million cycles.
- Fracture Repair: Lag screws in tibial plateau produce compression forces of 300–500 N. Cortical screws in distal radius stabilize osteotomies with load to failure > 150 N·m.
- Maxillofacial Reconstruction: Mini screws (1.2–2.0 mm) exhibit pull-out strength 100–250 N and torsional strength 0.4–1.0 N·m. Resorbable screws degrade over 12 months without adverse reactions.
- Pediatric Fixation: Resorbable polymer screws avoid secondary removal surgery; mechanical retention maintained for 6 months, degradation completing by 18 months.
Conclusion
Bone screws play a vital role in orthopedic fixation, combining advanced materials, precise geometry, and rigorous mechanical performance. Selection of appropriate screw type, material, and surgical technique is essential to achieve optimal stability and minimize complications. Adherence to international standards and thorough testing ensure consistent quality and biocompatibility. Continued refinement in design and material science will further enhance screw performance in diverse clinical scenarios.
FAQ on Bone Screws
What are bone screws used for?
Bone screws are critical components in orthopedic surgeries, primarily used for stabilizing fractures, spinal fusions, and reconstructive procedures. They provide the necessary fixation to allow for proper healing and stability of the bone.
What materials are bone screws made from?
Bone screws are typically made from biocompatible materials such as stainless steel, titanium, or polymer composites. Titanium is often preferred for its strength, lightweight nature, and resistance to corrosion.
What are the advantages of using bone screws?
Stability: Provide strong fixation for bone fragments.
Versatility: Can be used in various surgical procedures.
Minimally Invasive Options: Some screws are designed for use in minimally invasive surgeries.
Are there any risks associated with bone screws?
As with any surgical procedure, there are risks, including:
Infection
Non-union or malunion of bones
Screw loosening or breakage
Allergic reactions to materials
How long do bone screws remain in the body?
Bone screws can remain in the body indefinitely unless they cause complications. In some cases, they may be removed after the bone has healed, while in others, they are left in place.
What is the difference between bone screws and bone pins?
Bone screws are threaded fasteners that provide strong fixation, while bone pins are smooth rods used to hold bone fragments together but do not provide the same level of stability as screws.